About 18 doctors with the Center for Fetal Research – prenatal specialists, biomedical and embryogenesis engineers – led by CHOP’s Flake, Partridge and Davey, just published some cutting-edge research in Nature Communications (Nature.com; April 25, 2017). Dr. Alan Flake, Director of the Children’s Institute for Surgical Science at the Children’s Hospital of Philadelphia (CHOP), a Professor at the University of Pennsylvania School of Medicine, and Director of this Research project, along with co-authors Dr. Emily Partridge and Dr. Marcus Davey, put forth an article including first year study ‘Results’ concerning their ‘extra-uterine device;’ which many scientists and journalists are calling an ‘artificial womb.’ https://www.nature.com/articles/ncomms15112 (includes video-feed of breathing ‘fetal lamb kept alive an artificial womb)
This article has four more sections: Premature Statistics, Miscarriages, Extra-uterine System and Results (several pages), and Responses.
Some Premature Statistics
These authors of the article, ‘An extra-uterine system to physiologically support the extreme premature lamb,’ in their Abstract and Introduction cite numerous sources from various journals such as Seminars in Fetal & Neonatal and the New England Journal of Medicine, as well as from the CDC’s National Vital Statistics Reports (2015), to inform their readers on the seriousness and importance of premature births.
They state that, “In the developed world, extreme prematurity is the leading cause of neonatal mortality and morbidity due to a combination of organ immaturity and iatrogenic injury… In the United States, extreme prematurity is the leading cause of infant morbidity and mortality, with over one-third of all infant deaths and one-half of cerebral palsy attributed to prematurity. Advances in neonatal intensive care have improved survival and pushed the limits of viability to 22 to 23 weeks of gestation. However, survival has been achieved with high associated rates of chronic lung disease and other complications …particularly in infants born before 28 weeks.”
An April 25, 2017, MIT Technology Review article on this study, entitled, ‘Animals Set Survival Record Inside Artificial Womb,’ notes that “a full-term baby is born at 40 weeks… the work raises questions about whether artificial wombs could be used to extend the limits of fetal viability – that is, the ability of a fetus to survive outside its mother. In the U.S., 43 states have laws that ban abortions once a fetus is considered viable.”
The MIT article states that “Alan Flake says no technology can replace the earliest stages of development. ‘There are likely developmental requirements that we cannot replicate earlier in gestation, so we could create developmental abnormalities… we have no interest in creating more survivors with impaired quality of life. This is what we are trying to prevent’.”
I must remind the noble doctor(s) that they are not ‘creating’ and cannot ‘create’ or ‘replicate’ the miracle of ‘creating’ and hosting a human (or animal) zygote, blastocyst or early fetus. Even the agnostics at PBS’ NOVA conceded to the title ‘Life’s Greatest Miracle (Nov. 2001)’ on their DVD and Program which ‘tracked human development from embryo to newborn.’ I also remind the reader that when most woman discover they are pregnant – about six (6) weeks, the embryo is only about 1/5 of an inch; yet the heart is beating and brain is forming in the head; and that at the fetus only weighs an ounce at about 15 weeks or 3 ½ months. However, it is true that the very viable baby grows extremely rapid in the Second Trimester, from about 3 inches to about 10 inches between the 14th week and week 21 when premature babies regularly survive but many do often develop complications and conditions.
Now, one of the most recent National Vital Statistics Reports, Vol. 66, January 2017, revealed that “the preterm birth rate rose slightly in the United States for 2015, to 9.63% from 9.57% in 2014… infants delivered at less than 37 completed weeks of gestation… the early preterm birth rate (less than 34 weeks) was …2.76% in 2015… and the late preterm birth rate (34-36 weeks)… 6.87%.” The Report stated that Preterm 27 weeks and under was .68% of deliveries; early term (37-38 weeks) 25%, full term (39-49) 58.5%, late term (41) 6.5% and 42 weeks and over .4% of deliveries. It stated also that 3.98 million babies were born in 2015 in the U.S. and that 3.84 million were ‘singletons;’ 133,155 twins, 3,871 triplets, 228 quadruplets and 24 ‘quintuplets and higher.’

(above and below born at 22 weeks)

In theGuardian.com article (4/24/17) ‘Artificial womb for premature babies successful in animal trials,’ they report, “In the UK, around 60,000 babies – one in nine – are born prematurely each year needing specialist hospital care. The chance of survival at 22 weeks is close to zero, but the odds quickly improve for every extra day the baby stays in the womb. At 23 weeks the chance of survival is 15%, at 24 weeks 55% and at 25 weeks about 80% (this figure was just 53% in 2006). However, health outcomes have not improved as quickly as survival figures for very premature babies, with one study showing that 45% of children born before 26 weeks had serious cognitive impairments at 11 years.”
See also: Study shows earlier Fetus heartbeat

Miscarriages
Now, my wife and I have had 4 children and she had 3 miscarriages. Although, I believe the first was due to trying to soon after her being on birth control pills for several years, according to the Mayo Clinic about 10%-20% of pregnancies in the United States end in miscarriage; and according to the World Health Organization about 1 in 5 to 1 in 7 in various parts of Asia; and higher in parts of Africa. According to WebMd.com, ‘at least 85% of women who have miscarriages have subsequent normal pregnancies and births… but if you have two in a row, you should…’ see a doctor.
A substantial amount of both experts and non-experts on the subject believe that miscarriages are ‘natures’ or God’s way of taking a baby before it suffers significant disabilities. Nevertheless, in nearly every case the mother should not allow guilt or depression to affect her and her family’s future. My wife had Thyroid disorders, and many women do, and it is said to be a major cause of miscarriages; yet, I remind you we have 4 grown very ‘normal’ children. Other causes of miscarriage are diabetes (for most young women can be control by diet and exercise), lifestyles (drug, alcohol, smoking), and physical complications, such as uterine polyps or cervical incompetency; but a doctor such be able to notice and monitor such things.


Extra-Uterine System and Results
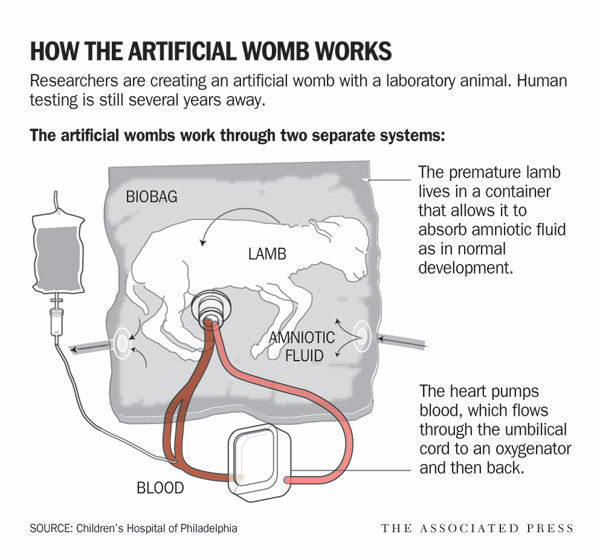
Flake, Partridge, Davey and company write in the Nature Communications article, “Here we report the development of a system that incorporates a pumpless oxygenator circuit connected to the fetus of a lamb via an umbilical cord interface that is maintained within a closed ‘amniotic fluid’ circuit that closely reproduces the environment of the womb. We show that fetal lambs that are developmentally equivalent to the extreme premature human infant can be physiologically supported in this extra-uterine device for up to 4 weeks. Lambs on support maintain stable haemodynamics, have normal blood gas and oxygenation parameters and maintain patency of the fetal circulation. With appropriate nutritional support, lambs on the system demonstrate normal somatic growth, lung maturation and brain growth and myelination.”
They continue, “The development of an ‘artificial placenta’ has been the subject of investigation for over 50 years, with only limited success. The primary obstacles have been progressive circulatory failure due to …oxygenator resistance and pump-supported circuits, the use of open fluid incubators resulting in contamination and fetal sepsis and problems related to umbilical vascular access… To address these obstacles we have designed a system consisting of three main components… a pumpless arteriovenous circuit, a closed fluid environment with continuous fluid exchange and a new technique of umbilical vascular access. Here we demonstrate that extreme premature fetal lambs can be consistently supported in an extracorporeal device for up to 4 weeks without apparent physiologic derangement or organ failure…”
“The initial series of experiments were performed in late gestational lambs (125-140 days of gestation; term = 145 days) and utilized an open fluid bath with continuous recirculation of an electrolyte solution… These studies lasted 23 to 108 h (hours) but were limited by sepsis and cannula-related complications.”
[Cannula is a thin tube inserted into a vein or cavity to drain off fluid or to induce fluid or medicine. Sepsis is a condition of the body responding to infection(s) to tissues and organs. Infections can be caused by bacteria, fungi, viruses or parasites. Here it is likely bacterial, and sepsis is caused by the body’s defense or immune system working overtime to fight the infection. It affects heart rate, blood flow and blood pressure and thus affects the oxygen and nutrient produced and flow and can lead to organ failure.]
They continue, “Our second design included a semi-closed fluid bath with continuous exchange of amniotic fluid, rather than recirculation. With the improved incubator, five experimental animals …ranging in age from 120 to 125 days of gestation were maintained on the system for 346.6±93.5 h, a marked improvement over the original design… one animal was maintained on the circuit for 288 h (120-132 days of gestation) and was successfully weaned to spontaneous respiration, with long-term survival confirming that animals can be transitioned to normal postnatal life after prolonged extra-uterine support. However, sepsis remained limiting in 3 of 5 lambs resulting in design of a closed fluid circuit (the Biobag).”
Continuing, “With introduction of the Biobag, pilot studies were performed with the aim to apply our system to earlier gestational fetuses. From the perspective of lung development, lambs at 100 −115 days of gestation are in the mid to late canalicular phase of lung development, which is the biological equivalent of the 22–24-week gestation premature human infant. However, in 110-day gestational age (GA) lambs with CA/JV cannulation, diminishing circuit flows and progressive oedema developed within the first few days… To offload the right atrium, we opted to utilize the umbilical vein (UV) for venous inflow to mimic normal fetal umbilical venous return and improve streaming of oxygenated blood across the foramen ovale.’
‘To avoid umbilical venous spasm, we advanced the umbilical venous cannula to a position with the tip just inside the abdominal fascia. CA/UV cannulation resulted in the stable support of five 106–113-day GA lambs for 13 to 26 days in the Biobag… All five lambs demonstrated long-term haemodynamic stability and stable circuit flows and oxygenation parameters… However, flow to the oxygenator in CA/UV lambs was well below the normal physiologic flow to the placenta… due to the inherently small-caliber carotid artery. The limiting problem… led to the …final device…”
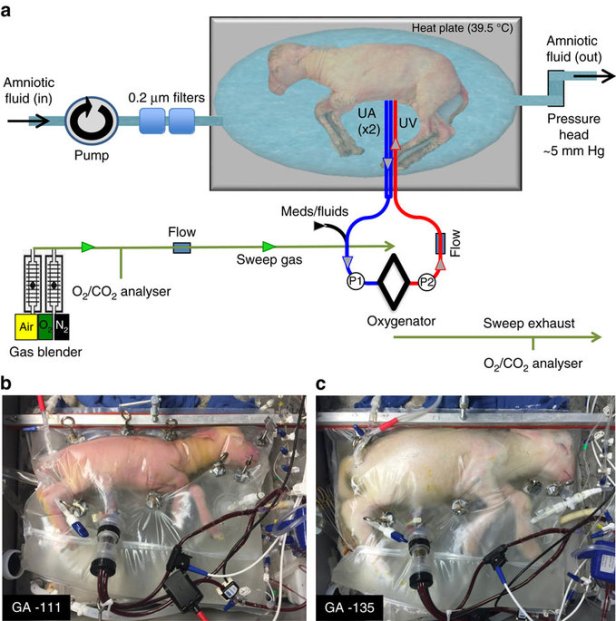
They continue, “From the inception of the study, we reasoned that a pumpless circuit—in which blood flow is driven exclusively by the fetal heart—combined with a very low resistance oxygenator would most closely mimic the normal fetal/placental circulation… To …address issues of sterility, size adaptability and efficiencies of space and fluid volume, a ‘Biobag’ design was developed—a single-use, completely closed system that minimizes amniotic fluid volumes and can be customized to more closely replicate the size and shape of the uterus. The Biobag consists of polyethylene film that is translucent, sonolucent and flexible to permit monitoring, scanning and manipulation of the fetus as necessary… After cannulation, the Biobag is sealed and transferred to a mobile support platform that incorporates temperature and pressure regulation, padding and the fluid reservoirs and fluid exchange circuitry…’
‘To more closely approximate flow dynamics in utero, carotid cannulation was abandoned in favor of double umbilical artery and single umbilical vein cannulation (abbreviated UA/UV) cannulation… The umbilical and venous cannulas are only 2 cm long, most of which is used for securing the cannulas, and therefore the interface is functionally end to end. Umbilical cord spasm was mitigated by a combination of topical papaverine administration, atraumatic operative technique and maintaining warmth and physiologic oxygen saturation of the umbilical venous inflow on initiation of circuit flow…”
“The combination of the pumpless oxygenator circuit, the closed fluid circuit and Biobag and umbilical cord access constitute our device. We have run 8 lambs with maintenance of stable levels of circuit flow equivalent to the normal flow to the placenta. We have run 5 fetuses from 105 to 108 days of gestation for 25–28 days, and 3 fetuses from 115 to 120 days of gestation for 20–28 days… The longest runs were terminated at 28 days due to animal protocol limitations rather than any instability, suggesting that support of these early gestational animals could be maintained beyond 4 weeks…”
“The nutrition provided via the circuit was based on substrate uptake of late-gestation fetal lambs, and hence consisted predominantly of carbohydrate and amino acid, with trace lipid. Our strategy in CA/UV and UA/UV lambs was to titrate dextrose and amino acid administration to levels of plasma glucose (<40 mg dl−1) and blood urea nitrogen (<30 mg dl−1) to avoid an osmotic diuresis and/or hyperosmolar state. Substrate tolerance generally correlated with oxygen delivery, and at relatively higher oxygen delivery, UA/UV lambs tolerated physiologic levels of substrate delivery and demonstrated growth comparable to breed-matched controls. From a qualitative perspective, there was obvious growth and maturation with prolonged runs. Animals opened their eyes, became more active, had apparently normal breathing and swallowing movements, grew wool and clearly occupied a greater proportion of space within the bags. The addition of insulin infusions in the last two lambs further improved substrate utilization and allowed administration of higher caloric loads with further enhancement of fetal growth.”
“Brains were grossly normal appearing… From a gross functional level, the UA/UV animals demonstrated normal or increased movement, sleep/wake cycles, intermittent breathing and swallowing and generally appeared comfortable and nondistressed.”
“A pumpless circuit powered by the fetal heart is not a new concept …the advantages include simplicity, absence of pump-induced haemolysis and the potential for at least some autoregulation of circuit blood flow. The disadvantages of pumpless systems include cardiac failure due to afterload imbalance if the circuit/oxygenator has supraphysiologic resistance, or the potential for high-output cardiac failure if the oxygenator has subphysiologic resistance. Most attempts have been limited by subphysiologic circuit flows and rapid haemodynamic decompensation despite the use of vasopressor support and other measures.”
“…A major concern in premature infants is intracranial haemorrhage, raising concern for the use of anticoagulation in extracorporeal support systems. We use substantially reduced heparin doses compared with conventional extracorporeal membrane oxygenation (ECMO) to maintain activated clotting times in the 150–180 s range… However, there is also evidence that germinal matrix haemorrhage is related to positive pressure ventilation, inotrope use and other interventions in the extreme premature infant. Thus, physiologic support in a extracorporeal system without ventilation or pressors may, in itself, reduce the likelihood of haemorrhage, making prediction of the impact of our system on intracranial haemorrhage difficult.”
“Finally, the umbilical cord offers the only physiologic vascular access for extracorporeal support for the fetus. The use of carotid arterial inflow or any other peripheral artery does not provide normal placental flows… While many investigators have utilized the umbilical vessels, most have placed their cannulas into the central vasculature to avoid umbilical vascular spasm. This is possible in sheep or goats, but not possible and would likely be hazardous for arterial cannula placement in the human fetus due to the tortuous course of the umbilical arteries and the large cannulas required. In contrast, we sought to take advantage of the natural resistance of the umbilical cord to occlusive events by developing an ‘end adapter’ design for our umbilical cannulation incorporating very short cannulas and a method for securing the cannulas to the umbilical cord. This avoids irritation of the vasculature or turbulence of flow at the end of the cannulas that might induce vascular spasm, erosion, aneurysm formation or thrombosis. It also allows a length of free umbilical cord between the cannulas and the fetus, preventing concern regarding decannulation or positional occlusion. As a result, we have been able to eliminate sedation during our runs and to maintain much more stable flows.”
“Clinical application of the technology will require further scientific and safety validation, and evolution and refinement of the device itself… In pilot studies on size-equivalent but developmentally far less mature lambs (85–95-day GA, 480–750 g), we encountered no limitations related to umbilical vessel caliber or oxygenator flows, confirming the technical feasibility of UA/UV cannulation at this size. We did see evidence of too much flow (300–350 ml kg−1 min−1) in our very early gestational, human-size-equivalent lambs resulting in hydrops and limiting our experiments to 5 to 8 days…”
| Their Conclusion (in part): “The initial clinical target population for this therapy will likely be the 23–25-week extreme premature infant. At the present time the morbidity and mortality of this population would seem to justify general application of this technology if it were proven to dramatically improve outcomes in clinical trials. Future developments may allow better prediction of those infants who are destined for extreme premature delivery…
Before 22–23 weeks of gestation, there are likely physiologic and technical limitations that will increase the risk and reduce the potential benefit of this therapy. Our goal is not to extend the current limits of viability, but rather to offer the potential for improved outcomes for those infants who are already being routinely resuscitated and cared for in neonatal intensive care units…” |
Responses
MIT Technology Review (4-25-2017) stated, “Partridge says placing babies inside the new device, which imitates a woman’s uterus, could lower the risk of death or long-lasting problems by allowing babies to finish developing. Researchers have been working on artificial wombs—or “ectogenesis”—for years. In 1996, Yoshinori Kuwabara of Japan’s Juntendo University successfully nurtured fetal goats in plastic chambers filled with amniotic-like fluid. But past efforts often harmed animals because they relied on mechanical pumps to circulate blood.
Flake says his team has been in discussions with the U.S. Food and Drug Administration and thinks the device could be tested in a neonatal ward within three to five years.
The authors plan to redesign the fluid-filled plastic enclosure so that it looks more like a traditional incubator and doesn’t alarm parents. “I don’t want this to be visualized as fetuses hanging on the wall in bags. That’s not the way this human device will look or work,” Flake says. The final system will be “parent-friendly,” he says.”
The Guardian reports (4-25-17), “Neil Marlow, professor of neonatal medicine at University College London, said that the latest study would be viewed as a significant step towards this goal. “This is real tomorrow’s world stuff,” he said. “They appear to have got lambs through four weeks which is a pretty momentous achievement.”
Colin Duncan, professor of reproductive medicine and science at the University of Edinburgh, agreed the study was a major advance, but was less optimistic than the authors about the timeline to clinic: “The use of steroid injections for women at risk of delivering a premature baby to help accelerate fetal lung development was discovered using sheep models. It has improved the survival of premature babies worldwide and made a huge impact on obstetric and neonatal practice. That treatment took well over 20 years to get into clinical practice.”
The Independent news source out of the United Kingdom wrote in common with the Guardian, but added that “Expert Professor Colin Duncan… said, ‘This research isn’t about replacing the womb in the first half of pregnancy. It is about the development of new ways of treating extremely premature babies.”
The National Geographic (4-25-2017) online article, noted “The average gestation time for humans is 40 weeks. But about 30,000 babies are born younger than 26 weeks old in the United States each year. Those pushing the limits of viability—22 to 23 weeks—typically weigh only about a pound and have less than a 50 percent chance of survival. Of those who survive, many have severe disabilities, including lung disease and cerebral palsy… If the new device succeeds, the parents of a premature baby might someday peer into an incubator that looks a bit like an aquarium. In the device, a premature infant is enclosed in a large, clear plastic bag filled with artificial amniotic fluid.”
Nationalgeographic.com continued, “The goal of any artificial womb system, G. Mychaliska (Uni. of Michigan Extracorporal Circulation Research Laboratory) says, is not to grow babies entirely outside the mother. “That’s a Matrix thing,” he says, referring to the 1999 film in which humans are grown in pods. “The whole point of the artificial placenta is to re-create the uterine environment for a period of time and allow the organs to develop to a point where the infant can tolerate postnatal life,” he says.”
Amelia Hope Burden (twin born 23 weeks)



The Truth Source Notes:
This research is needed and will likely be proved to save and better a myriad of lives. I only note for those that would try to experiment with such things for fetuses less than about 17 or 18 weeks; those well-meaning scientists 70 years ago in the Manhattan Project also said it was not their moral obligation to carry the weight of the future uses of their successful developments – some uses which greatly benefit cities and some which totally destroy them.
To the parent(s) of extremely premature babies, I imagine I would desire any reasonable help that offered hope to benefit my child; and my prayers are for your family and your baby. I only pray that you consider the uses of wisdom, knowledge, reason and understanding; as you, with hope and prayers, make your decisions forward. For those with the most extreme decisions to make; I offer the following:
Thought Process to a Most Difficult Decision
